Whether opioids are prescribed to treat chronic or acute pain, there are still risks associated with each treatment plan.1,2 Despite best efforts in educating and counselling patients on opioid use, accidents may still occur. Anyone taking opioids is at risk of having an accidental opioid poisoning.3
Both short-term and long-term opioid treatment plans carry similar risks. For example, patients may forget that opioids should not be mixed with alcohol or sedating medication, or they may have comorbidities that can increase their sensitivity to opioids, like hepatic, renal or lung disease.4 Also, accidents are not limited to the person that has been prescribed the opioids. Improper storage can lead to poisoning in young children or teens.5,6 A study conducted in Ontario between 2018 and 2019 showed that half of the high school students who had used opioids recreationally had obtained it from their home.7
For patients that have been on opioids for a long period of time, there can be additional risks to consider. Long-term exposure to opioids may cause tolerance to opioids, which may prompt patients to take more medication to achieve the same effect.8 Moreover, some patients may not be aware that their opioid tolerance can decrease in as little as 2-3 days after stopping their treatment.1 Stopping therapy for only a few days may increase their chances of experiencing an accidental opioid poisoning if they resume opioids.8
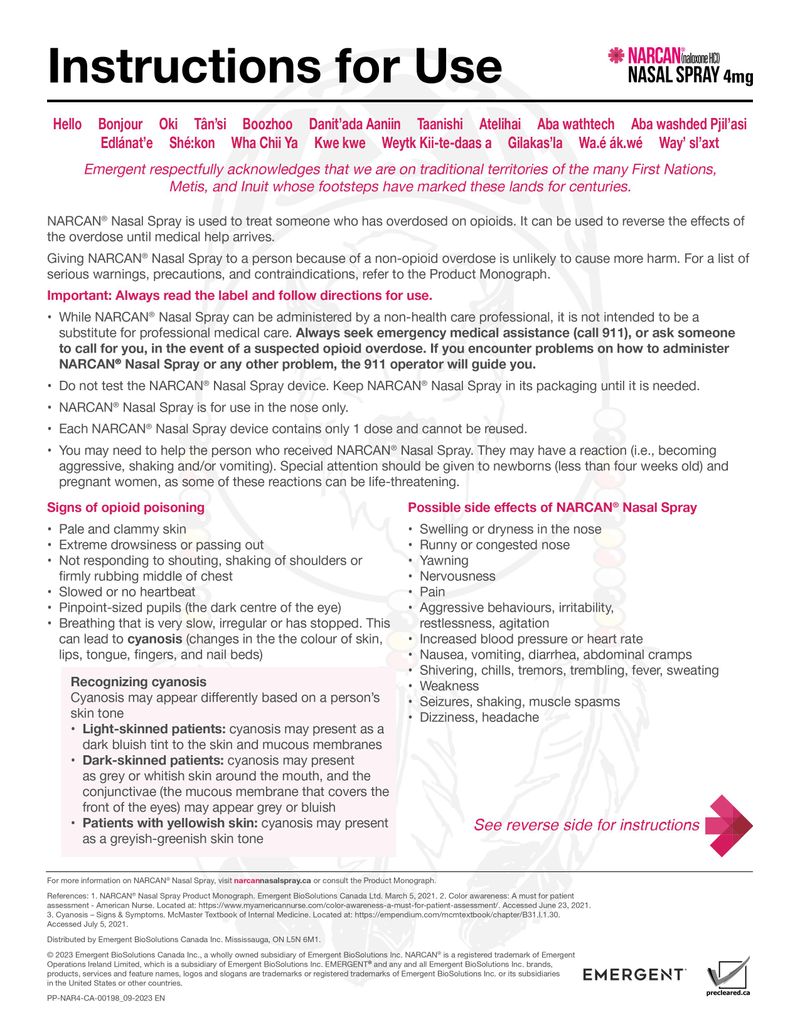
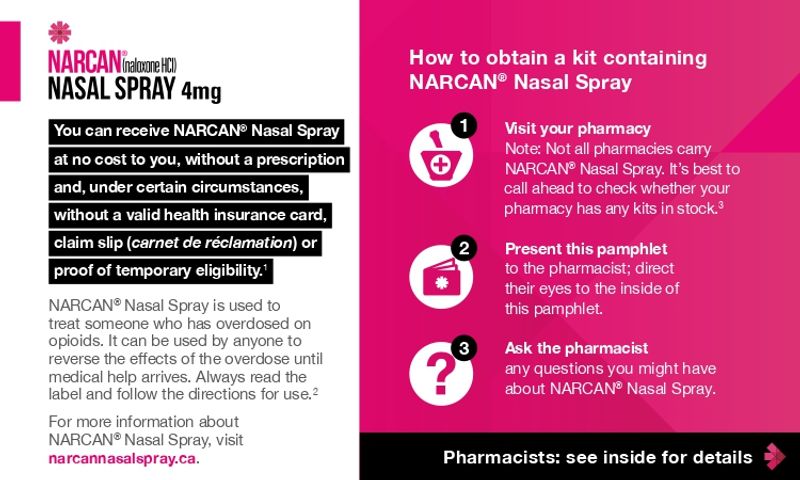
The risk of accidental poisoning can be difficult to predict.3 Every time you counsel your patients on opioid use, talk to them about a take-home naloxone kit, available in either a nasal spray form, like NARCAN® Nasal Spray, or an injection.1,3
When talking to patients who do not think they need NARCAN® Nasal Spray, here’s an example of what you can say:1,3,9
“I’ve explained the benefits and risks associated with your medication. As I mentioned, it is very important to take it as prescribed. That being said, accidents do happen and, because anyone taking an opioid is at risk of an accidental opioid poisoning, I would like to offer you NARCAN® Nasal Spray as a safety precaution. This is something I do for all of my patients; however, you are allowed to refuse it. Having naloxone in the home is similar to having a fire extinguisher in the kitchen. You hope you don’t need it, but you are prepared if you do.”
Make it part of your routine: offer NARCAN® Nasal Spray with every opioid prescription.
References: 1. Ontario Pharmacists Association. Pharmacist clinical tool for initiating naloxone discussions. Available at: https://opatoday.com/wp-content/uploads/Practice/Tools/Naloxone/Pharmacist-Clinical-Tool-for-Initiating-Naloxone-Discussions.pdf(Open in a new window). Accessed July 27, 2021. 2. Mayo Clinic. What are opioids and why are they dangerous? Available at: https://www.mayoclinic.org/diseases-conditions/prescription-drug-abuse/expert-answers/what-are-opioids/faq-20381270(Open in a new window). Accessed July 27, 2021. 3. Tsuyuki R et al. Canadian national consensus guidelines for naloxone prescribing by pharmacists. Canadian Pharmacists Journal. 2020;153(6):347-351. 4. Government of Canada. Opioid overdose. Available at: https://www.canada.ca/en/health-canada/services/substance-use/problematic-prescription-drug-use/opioids/overdose.html(Open in a new window). Accessed July 27, 2021. 5. Drug Free Kids Canada. Help your teens before they help themselves. Available at: https://www.drugfreekidscanada.org/prevention/drug-info/prescription-drugs/(Open in a new window). Accessed July 27, 2021. 6. Finkelstein Y et al. Overdose risk in young children of women prescribed opioids. Pediatrics. 2017;139(3): e20162887. 7. Ontario Student Drug Use and Health Survey. Drug use among Ontario Students. Available at: https://www.camh.ca/-/media/files/pdf---osduhs/drugusereport_2019osduhs-pdf.pdf(Open in a new window). Accessed July 27, 2021. 8. Government of Canada. About Opioids. Available at: https://www.canada.ca/en/health-canada/services/substance-use/problematic-prescription-drug-use/opioids/about.html(Open in a new window). Accessed July 27, 2021. 9. Mueller SR et al. Attitudes toward naloxone prescribing in clinical settings: a qualitative study of patients prescribed high dose opioids for chronic non-cancer pain. Gen Intern Med. 2016;32(3):277-283.
PP-NAR4-CA-00087_05-2024 EN